Getting Started
If you’re struggling to lose weight and are ready to make a change, you may be a candidate for bariatric surgery.
BMI and its Classification
The Body Mass Index (BMI) is one measure used to define overweight and obesity. It generally reflects the amount of excessive body fat although there are certain exceptions, such as the BMI of a woman who is pregnant, an athlete, a body builder or the elderly.
BMI does not necessarily take into account a person’s distribution of fat (abdominal vs. peripheral) and is not a good measurement of the metabolic activity of a person’s fat tissue.
Candidates for bariatric surgery must have a body mass index (BMI) of at least 35 with weight-related conditions or a BMI greater than 40 without weight-related conditions. Candidates must also have tried unsuccessfully in the past to lose weight through diet and exercise.
Candidates for bariatric surgery must have a body mass index (BMI) of at least 35 with weight-related conditions or a BMI greater than 40 without weight-related conditions.
Please Recalculate your BMI. There's been an issue with the information you provided.
Your Information:
Your Information:
Your Results:
Your BMI is , indicating your weight is in the category for adults of your height.
For your height, a healthy weight range would be from to pounds.
Talk with your healthcare provider to determine possible causes of underweight and if you need to gain weight.
Your Information:
Your Results:
Your BMI is , indicating your weight is in the category for adults of your height.
For your height, a healthy weight range would be from to pounds.
Your Information:
Your Results:
Your BMI is , indicating your weight is in the category for adults of your height.
For your height, a healthy weight range would be from to pounds.
People who are overweight or obese are at higher risk for chronic conditions such as high blood pressure, diabetes, and high cholesterol.
Your Information:
Your Results:
Your BMI is , indicating your weight is in the category for adults of your height.
For your height, a healthy weight range would be from to pounds.
People who are overweight or obese are at higher risk for chronic conditions such as high blood pressure, diabetes, and high cholesterol. Take this 1-minute prediabetes risk test.
| BMI | Weight Status |
|---|
| Below 18.5 | Underweight |
| 18.5—24.9 | Healthy |
| 25.0—29.9 | Overweight |
| 30.0 and above | Obese |
Recalculate BMI"My bariatric journey can be summed up in two words: life-changing. My surgeon has been a guiding beacon in a vast darkness of failed weight loss and downward spiraling of health issues."
Dennis Grove
starting weight 347 lbs | current weight 301 lbs
6 weeks post op
"Since having surgery I have stopped most medications, and no longer have blood pressure issues or high blood sugar. I have begun actually enjoying life and not just watching it pass by. I feel so amazing and never thought I would have such great results."
Brittany Wilcutt
starting weight 323 lbs | current weight 243 lbs
5 months post op
Our Approach to Surgery
Your life-changing, surgical weight-loss journey starts with 10 steps.
Step 1: Attend a Free Weight-Loss Information Session
One of the best ways to learn if you’re a bariatric surgery candidate is to attend one of our information sessions. Here, our team will discuss the bariatric surgery process with you, the risks and benefits of each type of weight-loss surgery, and answer any questions you may have.
Step 2: Call Insurance Provider to Check Coverage
Before scheduling your bariatric surgery, you should call your insurance provider to be sure the surgery is covered. You can give them the following CPT code of the procedure to find out if it will be covered.
- Roux-en-y Gastric Bypass: 43644
- Sleeve Gastrectomy: 43775
Step 3: Meet with the Nurse Navigator
The next step in your weight-loss journey is to meet with our nurse navigator to discuss your in-depth medical history, eligibility for surgery and what your insurance policy requires for surgery. If you’re eligible and approved by insurance, the nurse will help you set up additional appointments to begin your weight-loss journey.
Step 4: Meet with the Surgeon - Initial Appointment
After your consultation with the nurse navigator, you will meet with a bariatric surgeon. The surgeon will evaluate your condition, discuss your options, determine if surgery is needed and answer any questions you may have. If surgery is right for you, we’ll develop a pre-surgical plan that’s catered to your needs and fits your lifestyle.
Step 5: Meet with a Registered Dietitian
Your next step to bariatric surgery is education. The registered dietitian will provide you with resources and materials surrounding nutrition, exercise, instructions on how to prepare for surgery and postoperative materials for after surgery. The dietitian will also assess your readiness for surgery, ensuring it’s the right decision for you. Depending on insurance requirements, you will receive three to six months nutritional sessions with the dietitian to support you throughout your journey.
Step 6: Complete all Specialist Appointments
We want to be sure you are set up for success. Before your surgery is scheduled, you will meet with other specialists including an endocrinologist, pulmonologist, psychiatrist, cardiologist and a primary care provider to complete necessary testing and receive clearance for surgery.
Step 7: Receive Insurance Approval
After you have met with our team and received clearance for surgery from our specialists, we will sit down with you to make sure all requirements have been met for you to move forward with surgery. After review, we will need to receive insurance approval (pre-authorization) for your surgery. Your program records, office notes, program completion and approval request are provided to your insurance. Your surgeon’s office will notify you once your insurance is approved.
Step 8: Meet with your Surgeon – Pre-Surgery Appointment
Surgery is an exciting and life-changing step in your weight-loss journey. There are many different types of bariatric surgery, so we’ll make sure you know what to expect before, during and after and answer any questions you may have prior to your surgery.
Step 9: Surgery
Typically, you will be admitted to the hospital the morning of your surgery and will stay in the hospital for one to two days for monitoring. Your surgeon will decide when you are well enough to return to work, usually within two to three weeks.
Step 10: Follow-Up Care
While this may be the last step in our approach, consistent weight loss is an ongoing journey. And we’re still with you every step of the way. Our follow-up care is personalized to meet your needs, keep you on track and help you overcome any physical, emotional and mental challenges that may arise. Our team is always here to support and help you.
"My bariatric journey can be summed up in two words: life-changing. My surgeon has been a guiding beacon in a vast darkness of failed weight loss and downward spiraling of health issues."
Dennis Grove
starting weight 347 lbs | current weight 301 lbs
6 weeks post op
"Since having surgery I have stopped most medications, and no longer have blood pressure issues or high blood sugar. I have begun actually enjoying life and not just watching it pass by. I feel so amazing and never thought I would have such great results."
Brittany Wilcutt
starting weight 323 lbs | current weight 243 lbs
5 months post op
Types of Surgery
Cullman Regional’s Bariatric Center of Excellence offers weight-loss surgery options including sleeve gastrectomy, gastric bypass surgery (also referred to as Roux-en-Y procedure) and revisional bariatric procedures.
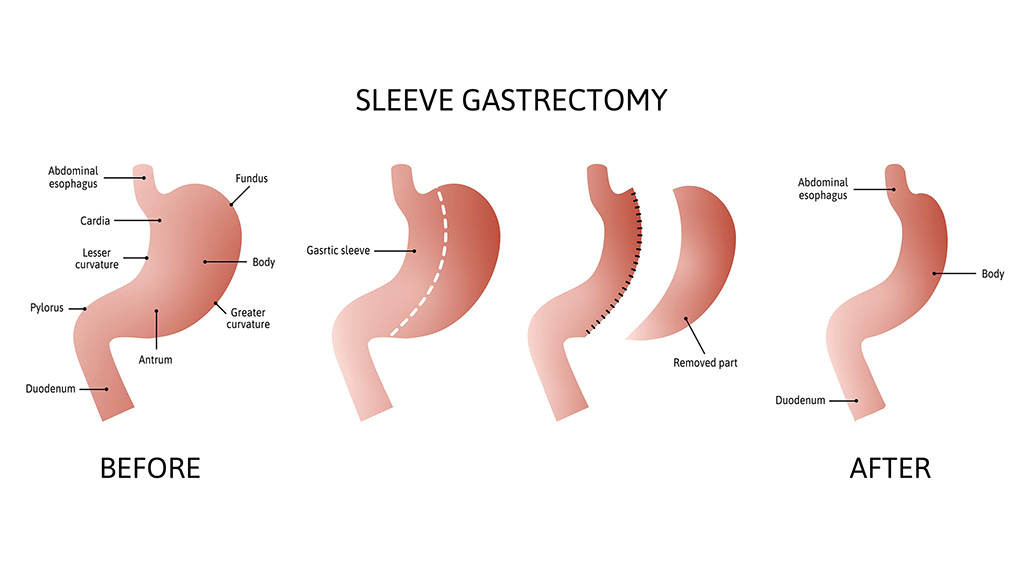
What is Sleeve Gastrectomy?
- A sleeve gastrectomy is a laparoscopic procedure in which the stomach is divided vertically and stapled so that 75 to 80 percent of the stomach is removed.
- The small part of the stomach that remains is shaped like a narrow tube (banana or a “sleeve”) and is connected to the intestine.
- The smaller stomach becomes the new “stomach” of the body and can only hold a small amount of food at one time.
- The small size of the new stomach restricts the amount of food patients can eat at one time by creating a feeling of fullness.
- A sleeve gastrectomy will not affect how the body absorbs food, so patients are less likely to experience nutritional deficiencies.
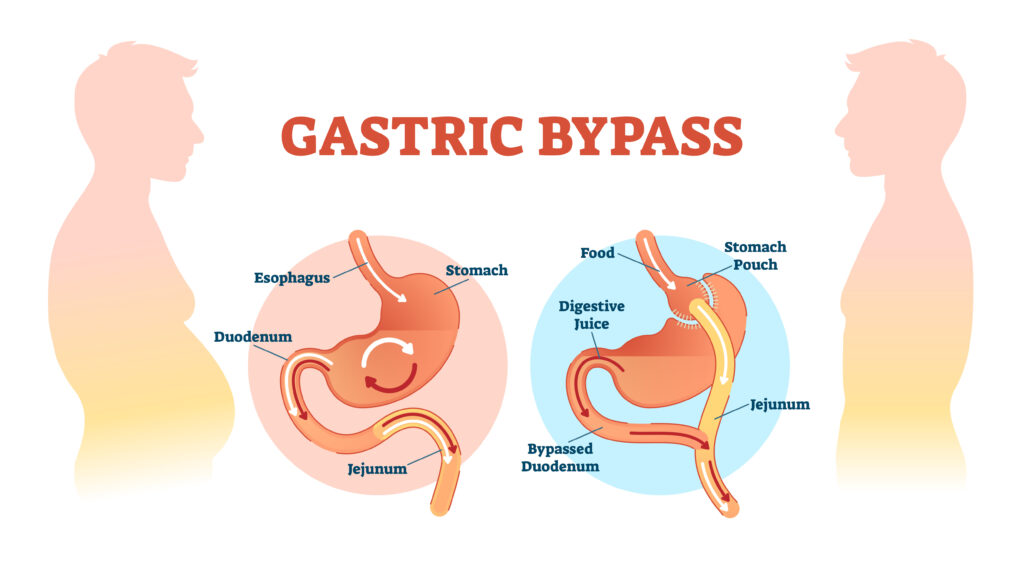
What is Gastric Bypass surgery?
- Gastric bypass surgery is a type of procedure in which the stomach is divided into a large pouch and a much smaller pouch about the size of a golf ball.
- The small pouch is stapled shut and divided from the large pouch.
- The small stapled pouch is then rerouted to a lower part of the small intestine, bypassing a portion of the upper small intestine.
- The small stapled pouch becomes the new “stomach” of the body.
- The small pouch can only hold about three to four ounces of food at a time, drastically limiting the amount of food you can eat in one sitting.
- The rerouting of the small pouch into the lower small intestine allows for the malabsorption of calories, spurring on more weight loss since fewer calories are absorbed.
What is a revisional bariatric procedure?
A revisional bariatric procedure is one where a patient’s first bariatric surgical procedure is being revised for various reasons. This may include conversion of sleeve gastrectomy to gastric bypass surgery, conversion of gastric band to sleeve gastrectomy, conversion of gastric band to gastric bypass surgery or resizing of the gastric pouch in gastric bypass surgery patients.
"My bariatric journey can be summed up in two words: life-changing. My surgeon has been a guiding beacon in a vast darkness of failed weight loss and downward spiraling of health issues."
Dennis Grove
starting weight 347 lbs | current weight 301 lbs
6 weeks post op
"Since having surgery I have stopped most medications, and no longer have blood pressure issues or high blood sugar. I have begun actually enjoying life and not just watching it pass by. I feel so amazing and never thought I would have such great results."
Brittany Wilcutt
starting weight 323 lbs | current weight 243 lbs
5 months post op
Getting Started
If you’re struggling to lose weight and are ready to make a change, you may be a candidate for bariatric surgery.
BMI and its Classification
The Body Mass Index (BMI) is one measure used to define overweight and obesity. It generally reflects the amount of excessive body fat although there are certain exceptions, such as the BMI of a woman who is pregnant, an athlete, a body builder or the elderly.
BMI does not necessarily take into account a person’s distribution of fat (abdominal vs. peripheral) and is not a good measurement of the metabolic activity of a person’s fat tissue.
Candidates for bariatric surgery must have a body mass index (BMI) of at least 35 with weight-related conditions or a BMI greater than 40 without weight-related conditions. Candidates must also have tried unsuccessfully in the past to lose weight through diet and exercise.
"My bariatric journey can be summed up in two words: life-changing. My surgeon has been a guiding beacon in a vast darkness of failed weight loss and downward spiraling of health issues."
Dennis Grove
starting weight 347 lbs | current weight 301 lbs
6 weeks post op
"Since having surgery I have stopped most medications, and no longer have blood pressure issues or high blood sugar. I have begun actually enjoying life and not just watching it pass by. I feel so amazing and never thought I would have such great results."
Brittany Wilcutt
starting weight 323 lbs | current weight 243 lbs
5 months post op
Why Cullman Regional Occupational Health
Cullman Regional provides the highest quality occupational health, worker’s compensation injury treatment, therapy, wellness services and more. We provide programs to serve your needs whether you are federally mandated or simply wish to provide a safer, healthier, more productive workplace for your employees.
Whether you need employee physical exams, screenings, education or work injury treatment, see us for a personalized plan. We’re here to support you and the wellness of your workforce with services at our clinic or on-site at your company.
- Work-related injury treatment
- DOT Physicals
- Pre-employment physicals
- Return-to-work physicals
- Drug screen collection
- Breath alcohol testing (BAT)
- Spirometry
- Audiology
- Ask about on-site & other services
- After-hours care coordination through Cullman Regional’s Emergency Department
Frequently Asked Questions
What is Occupational Health?
Occupational health is a field of healthcare made up of multiple disciplines dedicated to the well-being and safety of employees in the workplace. It has a strong focus on injury prevention and employee education. Occupational health services include employee wellness, pre-placement testing, occupational therapy, occupational medicine and more.
How does employee testing create a safer workplace?
When employees are validated as capable to perform their tasks through testing, the results include not only a safer workplace but one that’s more productive, with fewer work-related injuries and lower costs.
Does Cullman Regional offer on-site testing?
Our on-site occupational healthcare team can come to your workplace for a range of cost effective screening, testing, treatment, and prevention and job site assessment programs.
What are the benefits of using Cullman Regional?
- Our Occupational Medicine professionals provide best in corporate healthcare and employee testing services
- Occupational healthcare specialist teams available in our clinics or at your workplace
- Serving companies of all sizes
- Walk-in appointments available
- After-hours care coordination through Cullman Regional’s Emergency Department
If you or someone you care about is struggling with mental health issues, our professionals at Turning Point Health Center can help. We understand that stress, anxiety and other behavioral health problems can affect your relationships, your ability to perform daily activities and your overall health. Cullman Regional provides a wide range of outpatient mental health services to individuals with emotional, psychiatric, behavioral or chemical dependency related issues.
Conditions We Treat
Our team specializes in the following conditions for patients of all ages, including:
- Depressive disorders
- Post-Traumatic Stress Disorder (PTSD)
- Bipolar disorder
- OCD
- Insomnia
- Eating disorders
- Intellectual disabilities & behavioral problems
- Autism in adults
- Anxiety & panic disorder
- Traumatic brain injury disorders & related behavioral problems
- Personality disorders
- Sexual & gender identity disorders
- Impulse control disorders
- Adjustment disorders
- Post-partum depression
- Psychotic disorders, including schizophrenia
Office Hours
Monday – Thursday: 8:00 am – 4:00 pm
Friday: 8:00 am – noon
Location
1948 Alabama Highway 157
Professional Office Building 1, Suite 360
Cullman, Alabama 35058
Contact
Telephone: 256-735-5570
Fax: 256-735-5571
To request services or a visit from Pastoral Care:
- On campus: Dial “0” and ask the operator for chaplain services.
- Off-campus: Call 256-737-2000 and ask the operator for chaplain services.
Meet Our Team
Our full-time chaplaincy program has been serving patients, family and staff members for over 14 years.
Delbert Freeman, BA, MA, M.Div
Current Ministry: Hospital and Hospice Chaplain
Rev. Dudley Brock
Current Ministry: Pastor, Faith Cumberland Presbyterian Church
Rev. Tim Aris
Current Ministry: Pastor, Spring Hill Baptist Church
Rev. Jack Collins, BA, M.Div.
Current Ministry: Volunteer Chaplain
Rev. Raul Dominguez, BA
Current Ministry: Associate Pastor, Cullman First United Methodist Church
Dr. Edwin Hayes, BA; M.Div.; D.Min.
Current Ministry: Volunteer Chaplain
Rev. Ray Latham, BA
Current Ministry: Volunteer Chaplain
Rev. Eric Martin, BA
Current Ministry: Pastor, Seventh Street Baptist Church
Randy Sellers, BA
Current Ministry: Pastor, Mt Zion Baptist Church
Rev. Andrew Siegenthaler, BA, M.Div.
Current Ministry: Pastor, Christ Covenant Presbyterian Church
Hours
The Cullman Regional Chapel is open to patients and guests 24 hours a day, seven days a week. Chaplains are also available 24 hours a day, seven days a week.
If you wish to speak with a chaplain, ask any Cullman Regional staff member to contact the on-call chaplain.
Location of Chapel
Fourth floor of the main hospital,
next to the Critical Care Waiting Room
Request a Chaplain
On campus: Dial “0” and ask the operator for chaplain services.
Off-campus: Call 256-737-2000 and ask the operator for chaplain services.
Chaplain Services Request Form
Vascular surgery specializes in the care of arteries and veins which carry blood throughout your body. At Cullman Regional, our vascular surgeons offer screenings, testing and treatment to help you manage vascular conditions and resume an active life.
Our surgeons combine the latest in medical technology with the utmost personal attention to ensure that you receive the finest health care available. As experts in the treatment of a wide array of vascular diseases, our surgeons use medical therapies, minimally invasive catheter procedures and surgical reconstruction to keep your blood moving properly. Treatment can improve mobility, reduce pain, help wounds heal and restore you to the activities you love. Many vascular conditions can be treated in-office or with non-operative and/or minimally-invasive procedures.
Our Services and Procedures
Our team specializes in a variety of vascular conditions, including:
- Peripheral artery disease
- Atherosclerosis
- Carotid artery disease
- Lower extremity disease
- Varicose Veins & Spider Veins
- Abdominal aortic aneurysm (AAA)
- Renal artery stenosis
- Critical limb ischemia
- Thoracic aortic aneurysm (TAA)
- Blood Clots
Frequently Asked Questions
What does a vascular surgeon do?
Vascular surgeons are specialists who are highly trained to treat diseases of the vascular system. Your blood vessels –arteries carrying oxygen-rich blood and veins carrying blood back to the heart — are the roadways of your circulatory system. Without smoothly flowing blood, your body cannot function. Conditions such as hardening of the arteries can create “traffic jams” in your circulatory system, obstructing the flow of blood to any part of the body.
How do I know I need to see a vascular surgeon?
Typically, patients are referred to a vascular surgeon by their primary care physician. Sometimes patients become acquainted with a vascular surgeon after an unexpected event lands them in the hospital. You might be referred to a vascular surgeon if you see your regular doctor for pain in your legs, and learn that you have peripheral arterial disease, for example. If you are in a high risk category: are a smoker, diabetic, and/or have high blood pressure, you may be a candidate for starting a relationship with a vascular surgeon.
What are warning signs of vascular problems?
- Pain or tiredness in legs
- Burning or tingling in feet
- Sores or breaks in skin of legs and feet
- Aching in feet or toes when at rest
- Changes in skin color
- Buttock pain
- Decrease in skin temperature
How do I improve my vascular health?
- Don’t smoke or use tobacco.
- Eat a healthy diet low in cholesterol and saturated fat.
- Maintain a healthy weight.
- Exercise regularly to improve circulation.
- Don’t cross your legs.
- Take care of your feet.
How do I schedule an appointment with Dr. Miller?
Please call our office at 256-734-7850 to schedule your appointment today or schedule online, anytime, by clicking here.
Do I need a referral to be seen?
We will schedule all patients who call and request to be seen, however if your insurance requires a referral you will need to have that in file prior to your visit. Please check with your insurance for clarification.
Please note if your insurance requires a referral and it has not been obtained prior to your appointment, we may have to re-schedule your appointment.
When should I arrive for my appointment?
Please arrive at least 15 minutes prior to your appointment and please arrive 30 minutes prior to your appointment if you are a new patient.
For a procedure, you should arrive 30 minutes before your scheduled procedure.
What information do I need when I come into the office for my first visit?
Please bring the following:
- Your insurance card
- Driver’s license
- All you medications you are currently taking
- A list of your past surgeries, allergies and health history
What types of insurance do you accept?
We accept most insurance providers. We recommend patients contact their insurance company as each plan offers different levels of coverage. Please check the back of your insurance wallet card for contact telephone numbers.
Office Hours
Monday – Friday, 8:30 a.m. to 5:30 p.m.
Emergencies: If you need to consult with a doctor after regular office hours, you may call the Cullman Regional operator at 256-737-2000. The operator will assist you in reaching the surgeon on call.
Location
1930 Alabama Highway 157
Cullman, Alabama 35058
Contact
Telephone: 256-734-7850
Fax: 256-734-9633
Emergencies: 256-737-2000
Cullman Regional’s Social Services team is available to help families find the necessary resources to improve the life and living conditions for our patients. Our staff members are licensed social workers with more than 15 years of experience in the field.
Our Services
We help current Cullman Regional patients and their families with the following:
- Resource Information and appropriate referrals
- Discharge Planning
- Crisis Intervention
- Abuse/Neglect assessment and reporting
- Psychiatric referrals
- Substance abuse referrals
- Transportation/Housing issues
- Advance Directives
- Emotional Support
- Education
Frequently Asked Questions
How do I find a primary physician?
You may call the Cullman Regional Physician Referral line at 256-735-5600 or search online.
How can I arrange transportation to/from my doctor’s appointments?
Cullman Area Rural Transportation Services (CARTS) can provide transportation to local physician appointments for a nominal fee. For more information or to schedule a pick-up, call 256-734-1246.
How do I probate a mentally ill family member who is a danger to self and/or others?
The first step is to file a Report of Concern with Mental Healthcare of Cullman. Contact them at 256-734-4688.
How can I seek follow-up medical care when I have no insurance?
Good Samaritan Health Clinic serves the uninsured adult residents of Cullman County, Alabama by providing access to primary healthcare. Contact the Good Samaritan Clinic at 256-775-1389 or goodsamaritancullman.com for more information. Good Samaritan Health Clinic is located at:
401 Arnold Street, NE
Suite A
Cullman, AL 35055
Hours
Monday-Friday, 8 a.m. to 4:30 p.m.
On-call after hours and weekends as needed and appropriate
Location
Our services are available at the patient’s bedside.
Contact
Phone: 256-737-2450
Fax: 256-737-2374
If you or someone you know is in the hospital as an inpatient, chances are you or he/she may be seen by a hospitalist — a specialist in inpatient medicine who cares only for patients in the hospital. He or she typically spends most of the workday in the hospital and is more readily available to you than physicians who are seeing patients in their offices. The hospitalist has no responsibilities outside of the hospital, enabling him or her to focus exclusively on care for the hospitalized or acutely ill patients.
What Does a Hospitalist Do For You?
Most hospitalists are board certified in internal medicine (internists) or family medicine. They work alongside other specialists who may be involved in your care, ordering tests and procedures and monitoring your condition, ensuring a fast response or change of treatment if your condition changes. You may wonder why your primary care physician is not in the hospital to oversee your care, whether he or she knows you are in the hospital, and if he or she will be updated about your care. Hospitalists work with your physician to obtain important medical history and discuss treatment plans as necessary. Upon discharge, your physician will receive a complete summary of your hospital stay, test results and other relevant follow-up information.
Our Services
Services provided by our hospitalists include:
- Admission-to-discharge care of medical patients over 16 years of age
- Medical consultation on surgery, psychiatry and other non-medical services
- Critical care unit care for patients with a primary medical condition
- Admitting and caring for medical subspecialty cases with consultative back-up
Frequently Asked Questions
What is a Hospitalist?
A hospitalist is a specialist in inpatient medicine whose practice is dedicated exclusively to providing care to patients while in the hospital. This means that the hospitalist can focus all of his or her attention on patients who are hospitalized and is more readily available than a physician who is seeing patients in his/her office outside of the hospital.
Most hospitalists are board certified in internal medicine (internists) or family medicine. Some are medical subspecialists who have chosen to focus on inpatient hospital work, such as intensive care physicians (intensivists), lung doctors (pulmonologists) or kidney doctors (nephrologists).
Do hospitalists replace my primary care physician?
Hospitalists do not replace your primary care physician. They work with your physician and other specialists as needed to ensure that you receive the best possible care and treatment. The physicians communicate with one another and encourage patients to follow up with your primary care physician after discharge from the hospital.
How does my primary care physician know about my hospital stay?
Hospitalists at CRMC will work closely with your primary care physician, including notification of admission and discharge. Our hospitalists also help to ensure that patients follow up with your personal physician to promote continuity of care.
What are the benefits of hospitalist care?
Our hospitalists work as a team to provide 24/7 care to patients in the hospital. They are more readily available to respond to hospitalized patients’ needs that often include conditions, symptoms or situations that are unpredictable. Hospitalists are immediately available if a medical emergency or a change in your condition arises. They also will discuss your care with specialists as needed to create a coordinated care plan. They will review and follow up on test results, assess your response to treatment, and make care adjustments when necessary to facilitate a speedy recovery.
What should I do after discharge?
After you are discharged from the hospital, follow up with your primary care physician or other specialists as instructed. Your primary care physician will review your health status and reconcile your medication list to ensure a safe transition.
Hours
24 Hours a Day, Seven Days a Week
Contact
Telephone: 256-737-2000